Introduction
Welcome to the Vascular Society's information for medical students. This section includes information about vascular surgery as a specialty and career.
It also provides contact information if you need further help or advice regarding student matters such as arranging someone to talk to your society, attachments in Vascular Surgery, career advice etc...
Trainees in vascular surgery have their own society called the Rouleaux club which you can also contact for help and advice.
Reasons to be a Vascular Surgeon
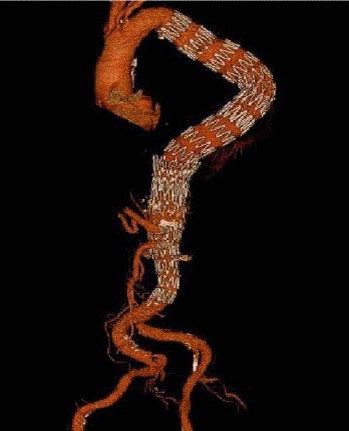
The treatment of vascular disease has undergone enormous change over the last two decades with the introduction of new technology that has revolutionised the specialty. For example, endovascular aortic stentr grafts for aneurysms, has hugely expanded the options for treating patients in a minimally invasive way.


Modern Vascular Surgery is a stimulating and challenging speciality. It comprises medical, surgical and endovascular techniques and covers different areas such as peripheral arterial disease (limb and carotids), aneurysmal disease, venous conditions, access fistulas, thoracic outlet syndrome, hyperhidrosis, and vasculitis. We treat patients from the 'head to the toes' so you carry out procedures on every part of the body. This is contrary to many other surgical specialities, which are becoming more and more focussed on specific anatomical areas of the body. We are the last real 'general' surgeons!
Vascular treatment is truly patient centered i.e. there is no "one size fits all" approach to anything we do. The treatment for the 55-year-old postman is different to the treatment of the 80-year-old astronomer with the same pathology. This means there is time to get to know your patients and do what is right for them, which leads to job satisfaction even on the most hectic day.
It is a unique specialty that requires both medical and surgical skills, both optimising patients for theatre, treating post-operative medical complications and deciding who should be treated medically from the outset. Understanding what each patient wants, and is willing in risk, is central to decision making and this often includes end of life care discusisions. Excellent communication skills are key.
Vascular Surgery is a specialty of both cutting edge endovascular technology and more established open operations. Many procedures are great to do and are technically challenging. This results in constantly feeling challenged when you intervene and not getting bored a decade into your career.
It also doesn't (normally) involve putting your finger or scopes into orifices, which the patients appreciate!
Patient numbers and new admissions are smaller than in other surgical specialities, therefore you get to know all of your patients well. You are able to offer a great service providing overall management and treatment. With the rise of diabetes, an ageing population, and the development of central trauma centres, job security is high.
This complexity means that most of vascular care is delivered by the vascular multi-disciplinary team involving medical colleagues in other specialities, nurses and allied healthcare professionals. Vascular units have a good multidisciplinary approach with good team working. The consultant involvement in patient care and teaching, for even minor operation, is very good. It is a very supportive and encouraging speciality. The new vascular curriculum has been put together by an exceptionally committed and enthusiastic group of vascular surgeons, who have an interest in ensuring delivery of excellent vascular training nationally.
There is also a very strong tradition of research in Vascular Surgery. We continue to look into the basic science of atheroma, the genomics of aneurysm disease and the role of inflammation in vascular disease. Many of the advances in endovascular technology have been pioneered by surgeons. The scope for innovation in technology through research has never been better than it is now. We wrestle with the place of vascular intervention in elderly multiply co-morbid patients, constantly evaluating the risk benefit profile for procedures in different groups of patients. This is stimulating, the stakes are high, life and limb are often in the balance.
‘All You Need to Know About Vascular Surgery’
The Society is proud to have launched a publication entitled All you need to know about Vascular Surgery. The book has been developed to provide a guide for medical students, early year doctors and allied healthcare professionals.
The book is available online, open access and available using the following link:
Annual Essay Competiton
The Rouleaux club runs annual essay competeion. All entrants are given free registration to the Vascular Society Annual Scientific Meeting (ASM) as well as the opportunity to take part in an introduction to vascular surgery training day (held in conjunction with the ASM).
The questions are announced in the summer and advertised on the Rouleaux Club and Vascular Society websites, as well as publicised via University Surgical Societies.
2023
The essay prize winners from 2023 have been published in the JVSGBI.
STUDENT CATAGORY
Is surgical bypass underutilised for patients requiring lower limb revascularisation?
Luke Davies, University of Bristol
DOCTOR CATAGORY
Discuss the role of Artificial Intelligence (AI) in improving current management of Abdominal Aortic Aneurysms (AAA)
Ishtar Redman, St George’s University Hospitals NHS Foundation Trust
2017
Matthew Machin, Imperial College School of Medicine, who won the best essay in the Clinical category; Kayani Kayani of Cambridge won the best essay in the Historical category ;and Jordan Green of Hull York Medical School won the best essay on the Research & Audit category.
Introduction to Vascular Surgery Course
This one day course is free to medical students and runs during the Charing Cross International Vascular Symposium (held in London in April) and the Vascular Society Annual Scientific Meeting (held in November).
This course is advertised on the Rouleaux Club and Vascular Society websites, as well as publicised via University Surgical Societies.
A career in vascular surgery
Frequently asked questions (FAQs)
1. What is Vascular Surgery ?
Vascular Surgery is the specialty that manages vascular disease outside of the heart and cranium. There is a small overlap with medical specialities who treat vasospastic and inflammatory conditions of the small vessels, but overall the majority of vascular conditions are managed by Vascular Surgeons. This includes both the arterial, venous and lymphatic systems. When we talk about managing vascular disease this covers prevention, medical treatment (anti-platelets, anticoagulants, lysis, statins, vasodilators) interventions (open surgery and endovascular catheter based interventions) surveillance and follow up. The curriculum is therefore broad and this makes for a varied specialty that maintains interest throughout your career.
2. Who carries out Vascular Procedures – Surgeons or Radiologists ?
A feature over the last 2 decades has been the revolution in technology that has changed the way we intervene for vascular disorders. Aneurysms are stented, veins are ablated, drug eluting angioplasty and stenting aims to improve the results for peripheral arterial disease. The modern vascular surgeon therefore needs to be able to carry out challenging open surgical procedures but also use imaging to guide catheter based endovascular procedures. Knowledge of ultrasound, cross sectional imaging and fluoroscopy are all required. The increased range of treatments expands the workload, and the demand for these interventions from an ageing sedentary population with diabetes and obesity is very high.
Various models exist internationally for how these procedures are delivered. Assessment and care prior to interventions is via referral to Vascular Surgeons. In some cases vascular surgeons also deliver any subsequent interventions whether open or endovascular. Interventional radiology (IR) can also deliver endovascular procedures. So in some cases patients will be referred to IR from vascular surgery for these procedures. Commonly for more complex and higher risk procedures both IR and the vascular surgeon will collaborate in the planning and performance of the procedure. Follow up and surveillance is supervised by the vascular surgeons.
There is therefore a care pathway for our patients that is largely supervised by Vascular Surgeons with elements delivered by both IR and vascular surgery. With the current high workload the deciding factor in who does what is often capacity in the system. In the UK therefore, it is likely that both specialties will need to contribute to the care of patients with vascular disease for the foreseeable future simply to deliver the workload required. In some other international health care systems with more capacity, resources and facilities, vascular surgeons may carry out both endovascular and open procedures in patients with vascular disease.
3. What is Vascular Surgery like for work life balance and family life ?
There is inevitably an emergency and urgent element to Vascular Surgery. Bleeding and acute ischaemia need treating quickly whenever they present. There is the potential for this to lead to individual surgeons working excessively out of hours.
The current solution to this is the development of larger teams, who truly share the out of hours work. Fewer, larger, vascular centres are now in place. A minimum standard is now a 1 in 6 on call rota, and 1 in 8 is becoming more common.
Such team working is the norm in many surgical specialties today. It has a lot of benefits for both the surgeons and more importantly patients. Vascular Surgery is now a specialty where this model of working is well developed. This has made a big impact on the working conditions for Vascular Surgeons. Teams work supportively and flexibly together, no individual surgeon needs to do excessive out of hours work. Work life balance and family life can easily be accommodated into such a working model.
There is a realisation in all surgical specialities that work life balance is central to a fulfilling career and Vascular Surgery is no different to any other specialty in that respect.
An important point to consider is that although out of hours work is inevitably unattractive, the acute problems that you need to deal with are often some of the most challenging and rewarding cases of your career. Exposure to some on call work will therefore be a positive part of your workplan.
4. What makes a good Vascular Surgeon? What attributes do I need?
4. What makes a good Vascular Surgeon? What attributes do I need?
Firstly, does Vascular Disease interest you? It is a common disease and it is important to treat it correctly to avoid serious adverse outcomes such as ruptured aneuryms, stroke and amputations. There are a number of treatments now and many are very successful.
Many of the attributes for a Vascular Surgeon are true for all forms of surgery. If you are practical and good at doing things you will make a good surgeon. You will work in a team, so if you get on well with people and communicate well that helps. As a Consultant people will look to you to lead the team. If you are comfortable with that your team will work well.
5. Why should I choose vascular surgery over other surgical specialties ?
Interest in Vascular Disease. A variety of work – arteries in different anatomical areas, open and endovascular procedures. Patients need medical as well as surgical care. A lot of your medical training will come in useful in your career as a Vascular Surgeon. If you are at all academic, Vascular Surgery has always been a very research strong specialty, there will be lots of opportunities to research or take part in clinical trials and audits.
6. What is a typical week like for a Vascular Surgeon ?
Most units are organised in networks with an arterial hub centre and spoke units where clinics and smaller procedures are performed but not major arterial work. Surgeons spend 4 days per week in the hub but will often spend a day each week out in a spoke unit.
All day operating list once a week – Stenting aneurysms, Carotid Endarterectomy, lower limb bypass are all common procedures. Hybrid procedures with some open surgery combined with an on table angioplasty or stent.
Out-patient clinics – 2 per week, half day each – 1 in hub, 1 in spoke
MDT meeting – half a day – review all imaging, discuss treatment with colleagues.
Local anaesthetic venous lists or access lists or peripheral endovascular list (angioplasty). Job plans often have a mixture of other smaller intervention lists such as these 1-2 half days a week.
On call – will average out over a 6-8 week cycle with roughly 1 day on call each week. You will be free of other commitments when on call.
Administration and professional development time – half day per week
Why did you choose Vascular Surgery ?
Often people choose vascular surgery because an enthusiastic surgeon acted as a role model and sparked their interest in the field. Involvement in a study or audit at an early stage often gets people interested. The surgery and procedures are great to do and getting a good result is very rewarding.
An attachment or “taster” sessions with a Vascular team are a good way to see if you like the specialty. Many medical schools will have these available for you to try. If not contact your local Vascular firm directly and they should be able to help. Contact the Vascular Society also, they can help put you in touch with a local team or surgeon to help you. We can also help find surgeons to come and talk to your student surgical society about a career in Vascular surgery and what is happening in the specialty.
